The latest figures show that general practice delivered a record 38.6m appointments in October 2024 (or more than 40m if you include COVID-19 jabs), that’s the highest ever one-month total on record. Additionally, primary care struggles with overwhelming demand and clinician shortages, and GP leaders warn that the pressure facing services is not sustainable.
So, what’s the solution? The challenges of expanding the workforce to increase capacity are widely acknowledged, so it is essential to focus on efficient strategies for either reducing demand or freeing up resources to address the persistent imbalance between growing demand and limited capacity in primary care. After years of time and money spent procuring, configuring, and embedding systems via frameworks and national programmes, it is clear that better use of such tools and technology is required. One of the most recent and impactful technologies is AI. To maximise benefits and ensure use and adoption at scale, we must ensure clinician and patient trust in the tools.
The importance of AI-powered telephone systems
Use of the digital front door is ever-increasing, but despite advancements, over two-thirds (68%) of patients continue to contact their GP practice via telephone as the first port of call. The shift from analogue to digital is something we all know is coming in the 10-year health plan, and as the most common mode of access is the telephone, it is clear that there is a fantastic opportunity to embrace the use of AI in primary care here. It’s also something that the Social Market Foundation has touched on recently in their report ‘In the blink of an AI’, with the recommendation of further integrating AI and automation into user-facing workstreams.
What benefits could AI in primary care bring?
The integration of AI in digital phone systems for primary care can offer transformative benefits, addressing some of the numerous pressing challenges. AI-powered features such as voice agents, call routing, speech-to-text, and automated signposting practices can alleviate the inbound pressure on call handlers while improving access and speeding up a patient’s time to care by offering an assessment at the first point of contact, in line with NHS national priorities.
Additionally, these streamlined processes reduce administrative burdens and repetitive tasks for staff, creating a more manageable workload and mitigating burnout. Together, these advancements pave the way for a more sustainable, patient-centered approach to primary care.
From X-On Health’s AI event held at The King’s Fund in November, speed and scalability emerged as two features of AI that would have the biggest positive impact, yet accuracy, usability and trust were significant factors to overcome. In my experience of deploying digital tools and redesigning automated patient pathways in primary care, building locally is key. Whilst we strive for standardisation, we know that local nuance remains between surgeries, and so tools and care pathways should be built around that local nuance to better offer equity of access to care, inclusion and personalised care. With AI, by ensuring accuracy and building trust, we can leverage the speed and scalability to deliver locally designed care models on a national scale.
How do we get patients and clinicians onboard?
The challenge is, how do we ensure that patients and primary care teams are harmonised with the progress to build their trust?
Building trust in patients is not simple, particularly considering digital poverty, which creates many disparities and makes it harder for people to access the very tools designed to help them. Patients value human interaction, especially when discussing health concerns, so AI tools must prioritise empathy in design and simplify communication. Data monitoring is key here and should be used to help provide evidence that effective digital tools will also improve access for all, including those who are less digitally able and require human contact.
Patients should not feel intimidated by AI, and it needs to be introduced straightforwardly, focusing on the benefits in relatable terms. Transparency of data usage is also vital; otherwise, we risk creating a two-tier system for those who trust data flows and storage and those who do not, which would also create further burdens for GP teams. Independent healthcare AI advisory companies, such as Curistica, are available to provide clinical and data governance assurances.
Patient empowerment means giving patients AI to self-serve for non-urgent needs. This will free clinicians to focus on more complex preventative care. If we can remove the demand before it flows into the practice, the burden will be eased immediately.
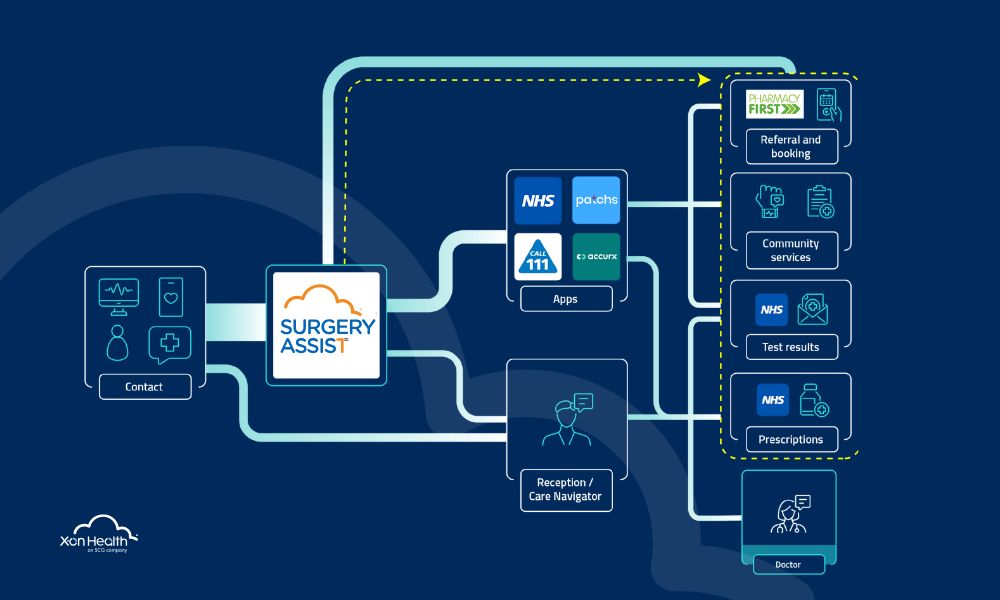
Locally trained AI agents, surfacing at the point of demand, offer GP surgery teams a layer of protection. At X-on Health, we are already advising clients to adopt a ‘bot’ first approach, in which AI assistants capture, manage, and redirect up to 40% of demand into non-GP services such as community service, PCN services, or self-service.
For clinicians and practice staff, AI in primary care should be seen as an opportunity to reduce pressure, not a threat to eliminate jobs. Clinicians are more likely to trust tools that they understand how to use, so time dedicated to training can demystify AI’s capabilities and limitations. The tech may be amazing, but it needs support to build in training for staff to make the best use of systems already in place and integrate tools such as Surgery Assist.
Take for example, Tudor Lodge Health Centre, a practice in South-West London that is an early adopter of Surgery Assist, an AI-powered tool that was applied as part of a wider Access Optimisation Service. The surgery has experienced 54% fewer calls in the 8am rush as a result. Applied nationally, it is estimated that this service could result in 9.1 million fewer calls received per month by GP surgeries.
Will AI in primary care live up to the hype?
One of the questions asked to the discussion panel at X-on Health’s recent AI in primary care event was, ‘Will it live up to the hype?’. AI is by no means a magic bullet, and Dr Keith Grimes outwardly expressed dismay at its underutilisation to date, then adding that if applied correctly, AI in primary care has the potential to move the industry forward beyond all expectations and solve several of its existing challenges.
As referenced by Patrick Denston, Digital Transformation Lead at Frimley ICB, at the same event, AI is a tool, not a solution and must be viewed as such. To my mind, it’s the correct approach, and AI should be viewed as an augmentation of our cognitive abilities which, when integrated into primary care workflows and digital products, can improve efficiencies and reduce the existing strain on the system. There is a crisis knocking on the door of primary care and the technology is needed now to help practices survive. Technology cannot simply be layered over inefficient processes. Instead, the two need to be addressed hand in hand so we can build trust and preserve the NHS in the AI era.
What are the next steps?
The overwhelming conclusion of last month’s event, taking into account macroeconomic changes, is that general practice is feeling ‘squeezed’ and more resource-stricken than ever before. The SWOT analysis, which all 50 attendees contributed to, highlighted that the benefits outweigh the risks regarding the application of AI in primary care. In fact, all attendees agreed that the adoption of AI tools was imperative to the survival of general practice.
While some GP partners have pushed on, spending a lot of time self-appraising AI products in pursuit of improved efficiencies to support their staff, there have been calls for the formation of an AI advisory board or list of approved AI suppliers to expedite procurement and adoption. It is also widely expressed that we must ensure we don’t introduce unnecessary bureaucracy, slow down the buying process, and delay the adoption of such time-saving tools.
The ‘In the blink of an AI ’ report supports the creation of a strong Digital Centre of Government in the Department for Science, Innovation, and Technology (DSIT) and recommends that it become a one-stop shop for all public sector AI and automation needs. It highlights tools that are already working and have been successfully implemented.
One thing is clear – if the NHS doesn’t work out how to become agile enough to embrace the technology and build trust quickly, then Google will do, as is clear from the Public First report, AI and the public sector, that was recently commissioned by Google Cloud.